Medicaid enrollment has grown considerably since the onset of the COVID-19 pandemic. As of May 2021, total Medicaid and CHIP enrollment was at 82.8 million, up by 11.5 million since February 2020. This safety net has been critical to the health and well-being of millions of people, such as those who experienced job loss, and loss of employer-provided insurance coverage, due to the economic effects of the COVID-19 pandemic.
As a condition of expanded federal funding, states had to agree to “Maintenance of Eligibility” (MOE) requirements to ensure the continuous coverage of certain Medicaid enrollees during the pandemic. These MOE requirements are active throughout the public health emergency, which has most recently been extended through mid-January 2022. This means that most state Medicaid redetermination processes have been on hold since March 2020, creating an enormous backlog of renewals.
Medicaid plans often struggle with keeping their members’ addresses up to date. Through Cotiviti’s Eliza member engagement solution, we know that 60% of enrollees consistently report not receiving their renewal notices in the mail. This could be because things get lost in transit, in the shuffle of a busy household, or maybe they’ve moved since applying for benefits. Transience has likely increased since the onset of the pandemic with individuals and families moving due to job losses, school closures, and housing instability.
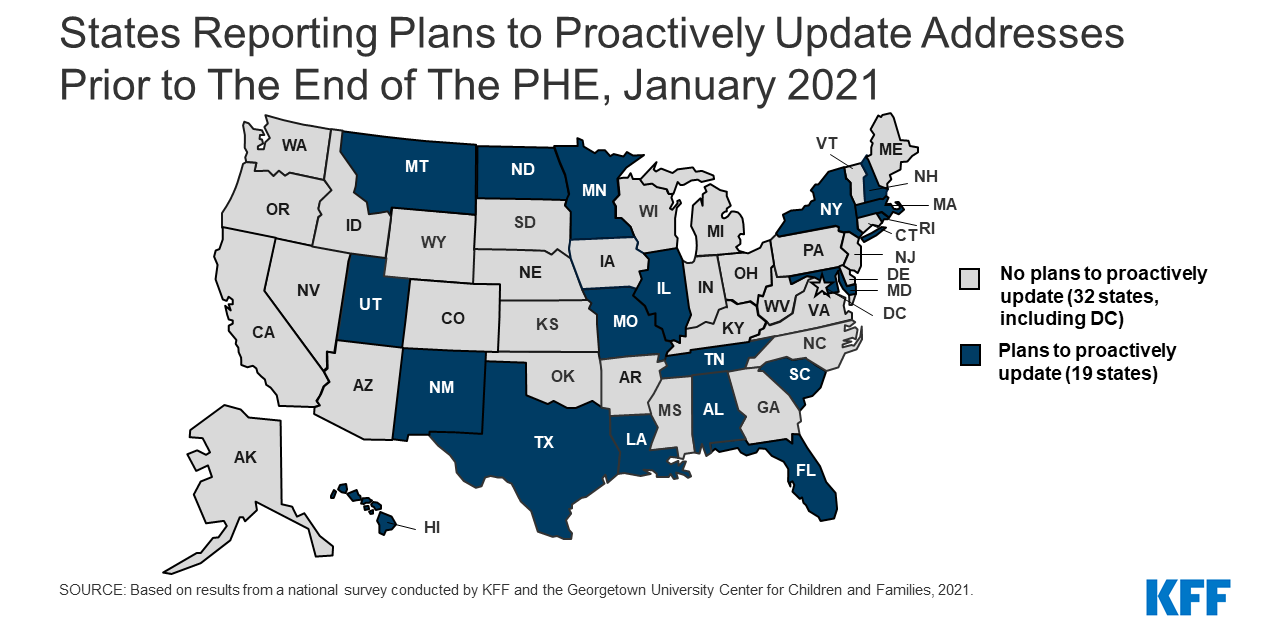
As states catch up on renewals in 2022 and the public health emergency eventually expires, plans should anticipate more Medicaid disenrollment and churn. Researchers at the Urban Institute predict that Medicaid enrollment will decline by 15 million people once the continuous coverage requirement of the Families First Coronavirus Response Act no longer applies. This includes nearly 9 million adults and nearly 6 million children. Some states have plans to proactively update addresses prior to the end of the public health emergency, but the majority of state Medicaid plans do not, according to a survey conducted by KFF and the Georgetown University Center for Children and Families.
Health plans, particularly those that are in states that are not updating addresses, can prepare for the reinstatement of redeterminations by collecting updated member contact information and communication preferences now. This will allow plans to notify members when it is time to renew benefits and avoid unnecessary loss of coverage.
Other actions Medicaid plans should consider include:
- Partnering with state Medicaid agencies to share updated member contact information.
- Offering members multiple ways to update their contact information including through a member portal, customer service, and secure communications such as interactive voice response and web surveys.
- Using every member interaction as an opportunity to make healthcare more accessible, such as highlighting your member portal, telehealth benefits, or how to access a free COVID-19 vaccination.
Eliza multi-channel engagement facilitates personalized interactions between health plans and their customers while gathering valuable member-reported data that can’t be found on an enrollment file or claim. We’ve helped Medicaid plans improve retention and revenue through administrative and medical expense savings by ensuring continuous coverage. Plans have gained more than 9% improvement in retention of those engaged.