Inpatient care is one of the most expensive types of healthcare services, where errors may delay payments, increase provider abrasion, and lower member satisfaction. But the complexity of inpatient claims often leads payers to bypass inpatient claim editing, resulting in millions of dollars in preventable overpayments for a single organization—and carrying high potential for provider abrasion when the plan seeks to recover those overpayments.
Most plans have relied exclusively on postpay claim review to catch inaccuracies in inpatient DRG review. In postpay, payers are typically able to recoup only about 70% of the identified overpaid amount at an additional recovery expense. In Cotiviti’s experience, the time to recoup value from postpayment identification can exceed 90 days (Figure 1).
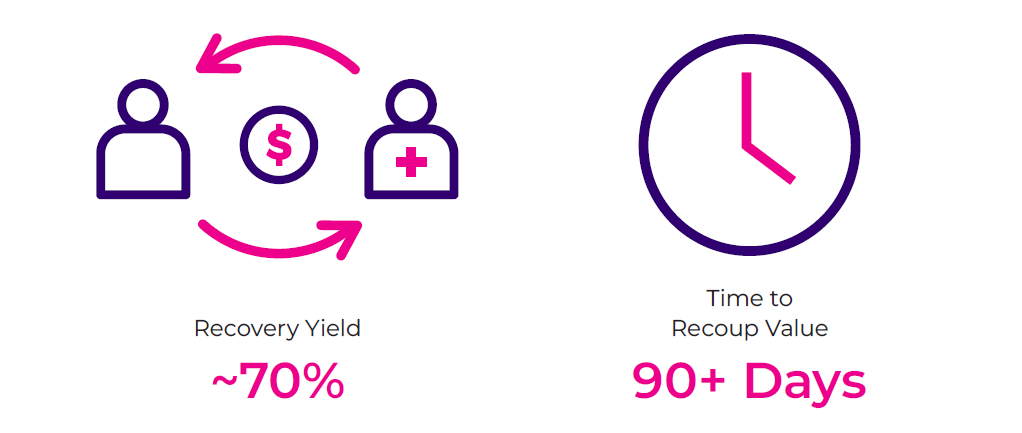
Figure 1. Challenges in optimizing value with retrospective DRG review.
Prepay claim review eliminates the pay-and-chase approach, where the plan pays the claim, identifies an overpayment, and is tasked with adjusting the claim and preparing an offset or pursuing recovery. Though retrospective review is a useful tool to report claim inaccuracies, implementing prepay review can reduce the financial and administrative burden of improper payments.
A comprehensive and tailored payment integrity program that monitors inpatient claim spend can protect member benefits and help ensure accuracy from the start. Inpatient payment integrity isn’t limited to reviewing DRG claims. By introducing new and expanded inpatient payment policy content to existing automated prepay final filter review practices, health plans can utilize full member contextual processing, looking across professional, outpatient, and inpatient claims.
Read Cotiviti’s new white paper for insight into how health plans can:
- Improve the efficiency and precision of existing postpay inpatient programs
- Apply prepayment integrity for inpatient claims to improve value
- Employ best practices to reduce provider abrasion
Seize new opportunities to improve your payment accuracy and learn how health plans have achieved greater payment accuracy through innovation and improved efficiency with prepay DRG review and expanded payment policy content.




