As COVID-19 cases and deaths surge in several hot spots across the United States, many individuals and organizations continue to ask, “What else can we do to help protect ourselves, our families, our communities, and our nation?”
Cotiviti’s efforts to aid in the pandemic response have confirmed three critical focus areas for policy makers and healthcare professionals:
- Improving testing capacity and processing time
- Informing the public on the risks of COVID-19 and the benefits of mitigation efforts
- Closing care gaps for those with chronic comorbid conditions
Continued insight from Cotiviti’s first response
When Cotiviti first launched the COVID-19 Outbreak Tracker in April, our goal was to help uncover areas of potentially hidden outbreak where community spread could be accelerating undetected due to severely limited COVID-19 testing capacity. In the early days of the pandemic, many symptomatic patients were being triaged and directed away from scarce testing resources, compromising the efficacy of available data. We observed that these triage procedures—which included telehealth visits, flu tests, and chest x-rays—were significantly delaying or preventing access to COVID-19 tests for many infected patients. We also recognized that Cotiviti had a unique view into these screening procedures through the millions of medical claims we process for over 60 percent of all U.S. healthcare transactions.
With this understanding, our data scientists analyzed, where permitted, relevant CPT and ICD-10 codes submitted from counties across the nation and searched for anomalies in influenza testing and diagnosis trends. From this analysis, we were able to accurately identify numerous hidden coronavirus outbreaks one to two weeks before they could be detected through limited COVID-19 testing. This early warning capability allowed us to inform policy makers, healthcare professionals, and individuals as they responded to the pandemic.
Our analytics team always expected and hoped this forecasting method would lose accuracy, which should happen once COVID-19 testing becomes accessible enough to replace screening procedures as the first step in evaluating symptomatic patients. However, despite a dramatic increase in testing capacity across the United States, our hidden outbreak tracker continues to yield greater than 80 percent accuracy and recently predicted major surges that have occurred in states such as Florida, California, and Texas.
This continued forecast accuracy is due primarily to two factors:
- First, most states still lack sufficient testing resources and capacity, and many providers, especially those in rural areas, continue to administer rapid flu tests as a triage procedure before sending symptomatic patients to distant testing centers.
- Second, the level of public adherence to social distancing guidelines and other protective measures like masks directly affects the spread of all infectious respiratory diseases. Any resulting changes in transmissibility can impact influenza and COVID-19 at the same time, but these changes can be observed in influenza trends weeks before they are observed in COVID-19 trends. This is due to a longer incubation period for COVID-19 and much longer delays in COVID-19 testing and recording of test results.
We continue to hope our accuracy will decline as this will be a clear indication that COVID-19 testing delays have been eliminated, and testing capacity is able to meet demand. We are encouraged by the steadily growing number of states with sufficient testing to suppress the virus and also by the increasing availability of rapid COVID-19 tests that can return results in minutes. These testing resources and capabilities, combined with effective programs for contact tracing and quarantine, give us a proven path to end the spread of COVID-19 and prevent future outbreaks.
Carefully navigating the path ahead
As we have monitored and updated our hidden outbreak tracker over the last few months, we also continued to research COVID-19. We have analyzed millions of longitudinal patient records to detect population health trends, including anomalies in the onset of acute and chronic conditions, the efficacy of treatments and interventions, and the impact of care quality, network performance, and social determinants of health on patient outcomes.
Through this research, we made many discoveries which have been further validated by other studies. We now know many critical details about COVID-19 clinical presentation, clinical course, clinical progression, and risk factors that we did not fully understand at the beginning of the pandemic. The following findings can be especially helpful to inform individual decisions about health and safety.
- Virus transmission is airborne and can occur indirectly. An infected person can spread the virus in aerosol by simply talking. Viable coronavirus can be rapidly dispersed through confined spaces and can linger in the air for minutes or even hours.
- The virus is a multi-system disease that can attack all vital organs causing brain damage, stroke, heart attack, and acute failure of lungs, liver, kidneys, and pancreas.
- Survivors may suffer permanent disability, chronic disease, and shortened life expectancy.
- Older populations are more likely to experience flu-like symptoms and viral pneumonia leading to acute respiratory distress and failure.
- Younger populations are presenting with symptoms of organ failure, stroke, and heart attack.
- Children are presenting with symptoms of severe autoimmune disease.
These findings are concerning, but social distancing and wearing a mask can greatly reduce the risk of spreading the virus. The head of the U.S. Centers for Disease Control and Prevention (CDC) recently stated that the pandemic could be brought under control nationwide within as little as four to eight weeks if all Americans wear a mask.
States like Hawaii that have taken aggressive measures to implement these guidelines have seen substantially lower infection, hospitalization, and mortality rates than those that have not. Other nations that have implemented these guidelines have eliminated major outbreaks, and New Zealand has even declared the virus eradicated. Better public understanding of the full risks of infection and the benefits of mitigation efforts can give us a way to move forward and end the pandemic.
Tracking COVID-19 health risk severity
Tracking and predicting the severity of COVID-19 cases is essential as we work to save lives and reduce the burden on healthcare systems. Much of the attention is focused on the daily number of new cases. Most reported cases are mild and do not require medical attention, but cases that are not mild present a much greater risk of long-lasting health problems or even death. Once patients start needing medical attention, they enter a funnel of clinical progression that can lead from primary care, to emergency care, to hospitalization, to intubation, and ultimately to death.
To avoid fatalities, we must look upstream in this clinical progression. While mortality and case fatality rates are important, they are lagging indicators and do not provide the predictive power or actionable insights of leading indicators. Leading indicators like quality of care for comorbid conditions are directly related to downstream deaths and provide a better window to inform decisions.
The United States currently has a relatively low case fatality rate of 3.5 percent compared to the fifty nations with the highest rates, which range from 3 to 15 percent and even as high as 28 percent in Yemen. This high variability in case fatality is due largely to accessibility and quality of care, which is an actionable insight into opportunities for preemptive interventions.
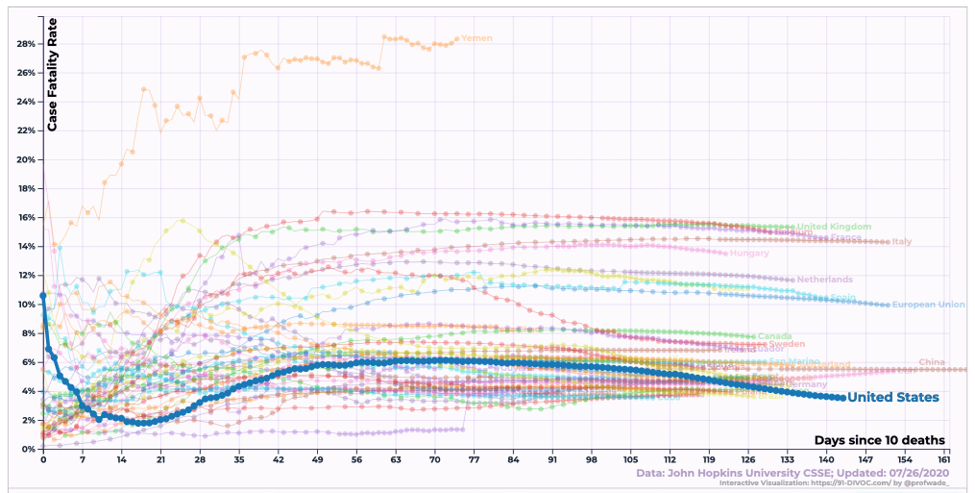
Figure 1. Cumulative COVID-19 case fatality rate.
(Data: Johns Hopkins University, Visualization: Wade Fagen-Ulmschneider, University of Illinois)
Despite being a recognized leader in biomedical research, medical technology, and hospital care, the United States is ranked 37th out of 191 countries for overall healthcare efficiency by the World Health Organization, which measures the relationship between responsiveness, outcomes, and cost. This 80th percentile ranking highlights the challenges we face with exorbitant healthcare costs and wide disparity in social determinants of health. It also underscores the problem with pooling all state data for a nation that has the world's third-largest population and land mass, diverse commercial healthcare, and a unique system of government that decentralizes many healthcare policies and regulations to individual states.
Pooling all state data can lead to sampling errors that blind us to the unique epidemiological trends and statistics in each state. These differences can produce outliers to nationwide trends as we saw early in the pandemic in New York, Washington, and California, and more recently in Florida, Texas, and Arizona. We even see extreme variability within states like New York, where inconsistency in quality of care between public and private hospitals has now been reported as a potential driver of mortality.
The United States cannot be viewed through a single lens. Public health policy, pandemic response, quality of care, and social determinants of health can be drastically different across states. These differences directly impact outcomes as we have seen in Utah, which has the lowest case fatality rate in the United States and is also home to many of the nation’s top-ranked hospitals and health systems; these include Intermountain Healthcare, an integrated managed care system, widely recognized as a leader in clinical quality improvement and efficient healthcare delivery.

Figure 2. Cumulative COVID-19 case fatality: select states and countries.
(Data: Johns Hopkins University, Visualization: Wade Fagen-Ulmschneider, University of Illinois)
To truly understand and predict the impact of COVID-19 on different populations, we must look beyond clinical risk factors and carefully analyze the ways in which chronic comorbid conditions are managed. Cotiviti is a leading provider of network performance, population health, and quality measures, which gives us unique insight into the impact of these factors on the risk of clinical progression and hospitalization for COVID-19.
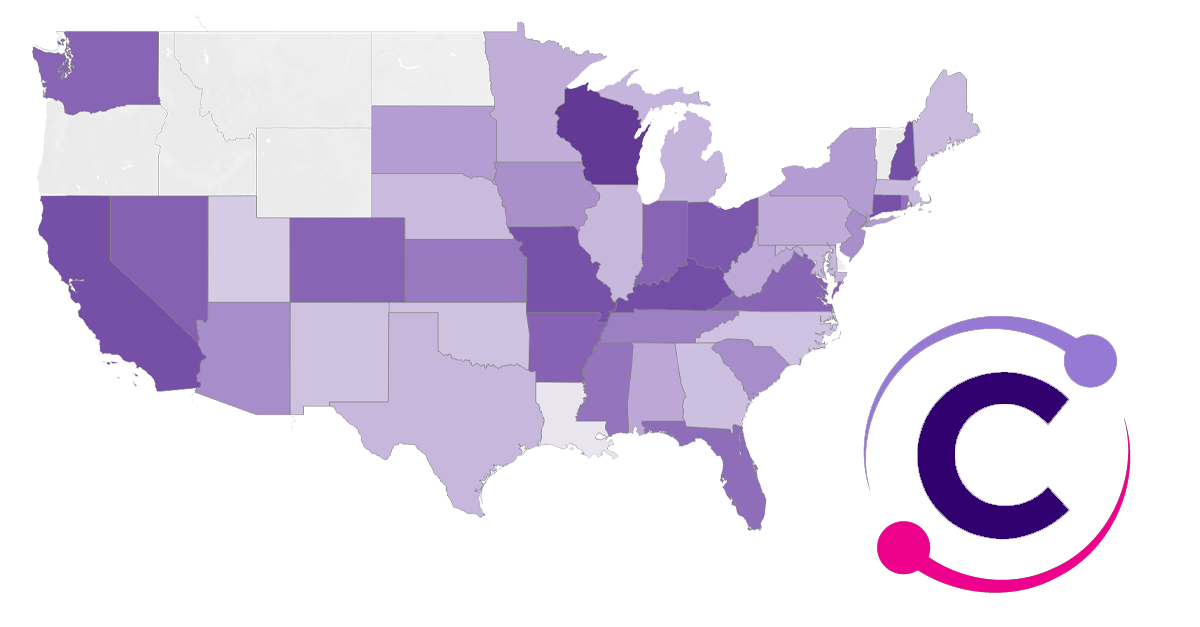
To further aid decision makers in pandemic response, we have recently published a new health risk severity tracker to share our insights. Darker states on this map indicate areas where populations are at greater risk of requiring hospitalization for COVID-19 due to the prevalence and management of comorbid conditions. These comorbidities include chronic conditions such as respiratory disease, cardiovascular disease, hypertension, and diabetes. These are conditions that require coordination between payers and providers to close care gaps and ensure patient adherence to care management plans.
Figure 3. Cotiviti’s COVID-19 health risk severity tracker.
There are several key takeaways from this map for all healthcare stakeholders:
- Higher-risk states may see greater mortality and increased strain on healthcare resource capacity.
- Governors in states with higher risk should anticipate and plan for a greater demand on healthcare resources and services.
- Payers and providers in higher risk states should focus on closing care gaps for patients with comorbid conditions and ensuring elective procedures for screening and care are not missed during the pandemic.
- Patients with comorbid conditions in higher risk states should understand their increased risk and take additional steps to social distance, wear a mask, and adhere to interventions and care management plans.
One of the most important findings from the health risk severity tracker is the connection between care gaps for chronic conditions and greater relative risk of severe infection. Patients are at much lower risk of requiring medical attention or hospitalization for COVID-19 in areas where these conditions are being managed through case managers to resolve care gaps or adherence issues. Unfortunately, we have observed in our data significant drops in the normal rates of screening procedures, preventative care, and maintenance care for those chronic conditions that greatly increase the risk of death from COVID-19.
Many patients and providers have cancelled or delayed screenings and wellness checks during the pandemic to lower the risk of infection. Despite the perceived risk of exposure to infection in a hospital or clinic, care facilities have strong protection in place to prevent infection. Community spread through social interaction without protective measures presents a higher risk of infection, and the risk of severe illness or death is much greater for those who skip the elective care visits and procedures required to properly manage chronic conditions. Payers, providers, and patients must work together—with informed guidelines and support from policymakers—to ensure we strike the right balance between social distancing and uninterrupted care for those most at risk.
Until a vaccine is available to all Americans, COVID-19 will remain with us and continue to threaten public health, strain our medical system, and take lives. As we promote and work toward on-demand testing capabilities, public adherence to preventative measures, and high-quality managed care, we can better protect ourselves, our families, our communities, and our nation.
For more resources, visit Cotiviti’s COVID-19 Resource Center to keep up with the latest pandemic news and its impact.