In the second episode of our “From the Trenches” podcast, we discuss the results of a new Cotiviti survey on the changing quality improvement landscape. As payers increasingly use quality data to drive performance improvement initiatives across their organizations, Cotiviti conducted the survey of health plan quality departments in late 2017 to determine how organizational shifts are affecting their strategy and planning.
Our guest on this episode is David Bartley, Cotiviti vice president of Quality and Performance. Listen here:
From the Trenches is a new podcast from Cotiviti, a leader in healthcare data analytics, exploring the latest trends in healthcare quality and performance analytics, risk adjustment, payment integrity, and payer-provider collaboration. Check out all our episodes in your browser, or subscribe on your smartphone or tablet with Apple Podcasts, TuneIn, Google Play, and Stitcher.
About our guest:
 As vice president of product at Cotiviti, David Bartley drives the product development strategy for Cotiviti’s Quality and Performance solutions, working closely with sales, client services, data operations, and development teams. David has more than 10 years of experience leading product development at a variety of leading healthcare companies, including Humana, Healthways, and eviCore. He holds a BA in economics from the University of North Carolina at Chapel Hill and an MBA from Vanderbilt University.
As vice president of product at Cotiviti, David Bartley drives the product development strategy for Cotiviti’s Quality and Performance solutions, working closely with sales, client services, data operations, and development teams. David has more than 10 years of experience leading product development at a variety of leading healthcare companies, including Humana, Healthways, and eviCore. He holds a BA in economics from the University of North Carolina at Chapel Hill and an MBA from Vanderbilt University.
Survey: the changing quality improvement landscape
Cotiviti fielded the brief online survey in the fourth quarter of 2017, requesting participation from health plans of all sizes. The survey had 68 respondents, which broke down into three approximately equal groups by job title: quality managers; director, VP, and above; and “other,” such as data analysts. Respondents also broke into approximately equal groups by health plan size: small (fewer than 100,000 members), medium (100,000 to 499,999 members), and large (500,000 members and greater). Medicare and Medicaid made up the bulk of respondents’ membership, although commercial membership was also represented.
Here is a preview of the results:
Q1: What is the relative importance of the following health plan initiatives to your organization (rank from 1 to 5)?
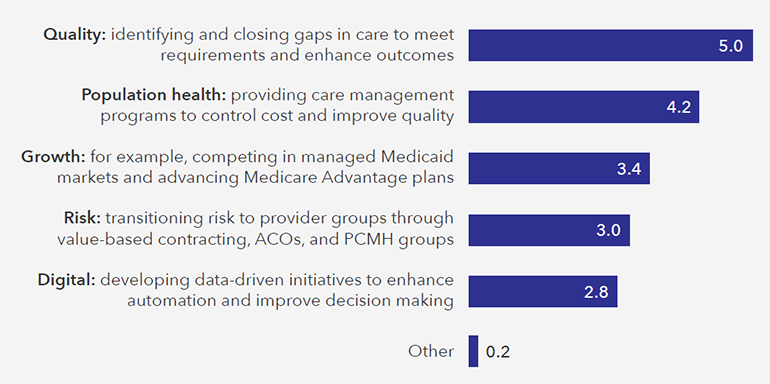
As Q1 reveals, closing gaps in care is still top of mind for quality teams, but respondents also indicated a significant awareness of population health initiatives that might not have been present as recently as five years ago, when quality improvement was viewed as more of an operational task performed for compliance and accreditation purposes. The high ranking for population health demonstrates the pressure that quality teams are receiving from groups both inside and outside of the health plan. In the context of cost control and quality improvement, both care management and provider network management teams are interested in quality data to better understand cost, utilization, and quality trends and corresponding improvement opportunities.
Another key takeaway is the relatively low importance respondents placed on both transitioning providers to risk-based arrangements and developing data-driven initiatives. While both are major topics of conversation in the industry, they aren’t as much of a focus for health plans yet, at least from the quality improvement team’s perspective.
Interested in reading the rest of the survey results and the insights we offer from both Cotiviti and health plan experts? Download the full white paper from our Resource library.
Podcast music credit: "Inhaling Freedom" by Nazar Rybak, via HookSounds.